If you've come here looking to learn more about patient health questionnaires used to assess mental and behavioral health disorders, you're in the right place. This blog provides information that helps answer the common question "What is a patient health questionnaire?" We'll discuss one of the most common patient health questionnaires and how it's scored and then briefly touch on a popular variant of this patient mental health screener.

More importantly, though, we'll provide an overview of why commonly used patient health questionnaires are coming up short. We'll conclude the piece by sharing some of the key qualities that providers should look for when choosing a better alternative to these flawed solutions.
Patient Health Questionnaire: Defining the Concept
Despite sounding like a broad concept that could apply to nearly all areas of health and wellness, the term "patient health questionnaire" is typically associated with mental and behavioral disorders. And you'll often see the concept treated as a proper noun and thus capitalized (i.e., Patient Health Questionnaire).
Why is that the case? To answer this question, we'll need to step back for a moment and briefly discuss the Primary Care Evaluation of Mental Disorders (PRIME-MD).
What is PRIME-MD?
Generally speaking, PRIME-MD is intended to be a diagnostic tool for common mental disorders. More specifically, the PRIME-MD is a two-stage system comprised of a patient screener typically with around 30 yes/no questions for patients to answer and a clinician evaluation guide, both of which are intended to help improve the diagnosing of five types of mental disorders:
- depressive,
- anxiety,
- alcohol,
- eating disorders, and
- somatoform, pertaining to somatic symptom disorder, which occurs when an individual feels extreme, exaggerated anxiety about physical symptoms.
The PRIME-MD was developed in the mid-1990s through funding from one of the largest pharmaceutical companies — one that just happens to develop and manufacture antidepressant drugs.
When using the PRIME-MD screener and evaluation guide, which provided clinicians with follow-up questions to ask patients based upon their screener responses, took more time than clinicians wanted to spend on diagnosing mental disorders, the PRIME-MD as a standalone tool was largely abandoned.
What is the Patient Health Questionnaire?
Now that we have a general understanding of PRIME-MD, we can look more closely at the concept of the "Patient Health Questionnaire," often referred to with its acronym of PHQ. The PHQ is a self-administered version of the PRIME-MD screener.
The three-page PHQ asks patients to speak to a number of potential mental health problems, signs, and symptoms they may be experiencing concerning the five modules (i.e., classes) of disorders noted above. While some questions ask patients to answer with a yes or no, others ask patients to assess how much and how long a problem "bothered" them.
Once completed, a clinician is supposed to review the questionnaire, focusing on those questions with positive responses, and then apply diagnostic algorithms, which are included and abbreviated at the bottom of each of the three pages.
In the late 1990s, one of the modules from the PHQ was broken out, which led to the creation of perhaps the most used mental health screening tool: the PHQ9.
What is a PHQ9 and How is it Scored?
What is the PHQ9? It's essentially the depression module of the longer, full PHQ. It asks patients to indicate how much they have been bothered by nine items over the previous two weeks. Those items are as follows:
- Little interest or pleasure in doing things
- Feeling down, depressed, or hopeless
- Trouble falling or staying asleep, or sleeping too much
- Feeling tired or having little energy
- Poor appetite or overeating
- Feeling bad about yourself — or that you are a failure or have let yourself or your family down
- Trouble concentrating on things, such as reading the newspaper or watching television
- Moving or speaking so slowly that other people could have noticed; or the opposite — being so fidgety or restless that you have been moving around a lot more than usual
- Thoughts that you would be better off dead or of hurting yourself in some way
For their responses, patients can choose from:
- Not at all
- Several days
- More than half the days
- Nearly every day
If a patient indicates they experienced any of the problems, they are then asked to speak to how difficult the problems made it for the patient to work, take care of home responsibilities, or get along with others. This is sometimes referred to as the 10th item of the PHQ9.
How is the PHQ9 scored? Once completed, answers of "Not at all" are scored 0; answers of "Several days" are scored 1; answers of "More than half the days" are scored 2; and answers of "Nearly every day" are scored 3. Thus, the PHQ9 total score for the nine items ranges from 0 to 27.
The National HIV Curriculum summarizes how clinicians should interpret the final score and the proposed treatment actions as follows:
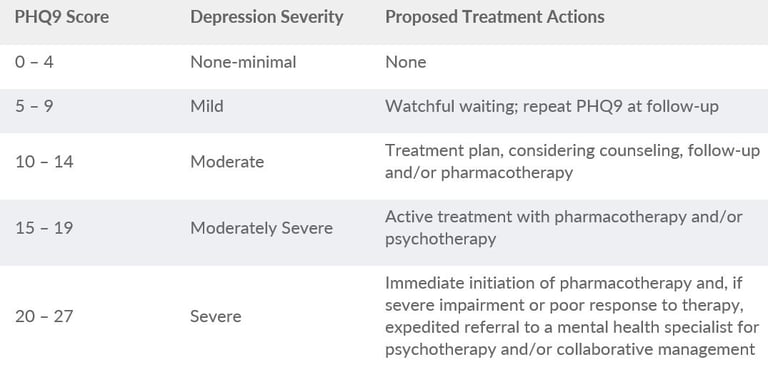
Unfortunately, as we will discuss momentarily, this mechanism for interpretation and action is inadequate for meeting patients' needs.
What is the PHQ2?
A tool related to the PHQ9 is the PHQ2. What is the PHQ2? Sometimes described as the "ultra-brief depression screening," it's simply the first two items from the PHQ9:
- Little interest or pleasure in doing things
- Feeling down, depressed, or hopeless
The PHQ2 is scored the same as the PHQ9, with patients who screen positive on the PHQ2 expected to be further evaluated using the PHQ9.
PHQ: The "Problem" Health Questionnaire
As we stated at the beginning of this blog, the patient health questionnaires increasingly relied upon and often treated as the "default screeners" can cause more harm than good for patients and clinicians eager to help patients get the most appropriate and timely treatment. There are several reasons why, including the following:
- These patient health questionnaires frequently fail to provide practitioners with an accurate diagnosis. This can delay the ability for mental and behavioral health patients to receive the care and support services they need and may lead to patients receiving services and medications that make a condition worse.
- Tools like the PHQ9 and PHQ2 are designed to identify symptoms or a group of symptoms for few conditions. This often leads a practitioner to predetermine the potential diagnosis based upon the tool being used. A diagnosis bias at the beginning of the patient assessment process can easily lead a patient down the wrong treatment path.
- Patient health questionnaires, which are intended as screening tools, have become diagnosis tools and increasingly therapeutic decision-making (e.g., prescribing) tools. But when the diagnosis is wrong or does not take into consideration other critical factors, patient harm can be significant.
We know that the patient health questionnaires largely in use today are coming up well short of their intended purposes when we look at the concerning state of mental healthcare today. Consider just the following statistics:
- Providers misdiagnose major depressive disorder 66% of the time.1
- Providers misdiagnose generalized anxiety disorder 71% of the time.1
- About 95% of people are not receiving appropriate screening.2
- The average delay between symptom onset and treatment is 11 years for bipolar patients.3
- People with depression miss an average of 27 days of work annually.4
Choosing a Better Patient Health Questionnaire
Fortunately, while the tools like the PHQ, PHQ9, and PHQ2 are often viewed as the default, they are not the only option for providers. Even better news: Some of the alternatives available can help providers improve patient care while also potentially adding revenue.
Here are some of the recommended criteria when evaluating behavioral health tools:
- Comprehensive — To strengthen support diagnosis accuracy, the assessment solutions you use should rely upon clinical interviews that screen for multiple disorders simultaneously.
- Clinically validated — When researching alternative assessment solutions, look for those that have been cited in well-established publications, clinical trials, and studies.
- Independent — Knowing the source for the assessment and screening solutions you use is essential. There is inherently room for bias when using assessments funded by a company or organization that may have a financial interest in how the solutions dictate patient care decisions.
- Digital — The demand for virtual mental healthcare is rising fast. If you intend to provide services using telehealth, paper-based assessments will hinder effectiveness and efficiency. Accommodating virtual mental healthcare for patients requires digital assessment tools.
- Reimbursable — The available time for clinicians to spend with their patients is at a premium. Ensuring you can bill for mental healthcare services is an important consideration for the short- and long-term viability of many organizations. The right solution can help you get paid for screening, diagnostic interviews, and/or monitoring.
- Easy to use — Another way to maximize the time available for patients? Choose solutions that support fast completion times and help providers reach an accurate diagnosis more quickly, all without harming care quality or the patient experience.
If you're interested in learning more about the challenges and opportunities around mental healthcare today, you won't want to miss "The Second Pandemic of Mental Health: An Expert Panel Discussion." This complimentary webinar is scheduled for August 17 at 4:30 EDT. Learn more about and register for the program here.
References:
-
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3184591/
- www.psychiatry.org/newsroom/news-releases/depression-screening-rates-in-primary-care-remain-low
- www.nami.org/NAMI/media/NAMI-Media/Infographics/NAMI-Mental-Health-Care-Matters-FINAL.pdf
- https://sapienlabs.org/mentalog/the-cost-of-poor-mental-health-in-the-workplace/





.png)








